Arterial hypertension—commonly known as high blood pressure—is a chronic condition defined by persistently elevated arterial pressure above 140/90 mmHg, affecting the heart and blood vessels and increasing the risk of cardiovascular events. It often has a multifactorial origin, with risk factors including genetic predisposition, lifestyle and metabolic factors (such as obesity and diabetes), chronic stress, and kidney disease; underlying mechanisms also involve vascular dysfunction and systemic inflammation.
Standard care—lifestyle changes and medication—remains the foundation of blood pressure control. Alternative treatments for hypertension are also being explored in research settings for selected patients. Stem cell therapy for high blood pressure is one such add-on approach, aimed at supporting vascular health, improving endothelial function, and lowering inflammation to help achieve better control alongside conventional therapy.
Arterial Hypertension Explained
Arterial hypertension refers to chronically elevated pressure in the arteries—the vessels carrying blood from the heart to the rest of the body.
What “Arterial Hypertension” Means in Everyday Clinical Practice
Blood pressure regulation is influenced by many interacting factors. These include genetic predisposition, neurohormonal mechanisms, vascular properties, and behavioral factors such as diet, physical activity, body weight, and stress. Different combinations of these influences can lead to a persistent increase in arterial blood pressure.
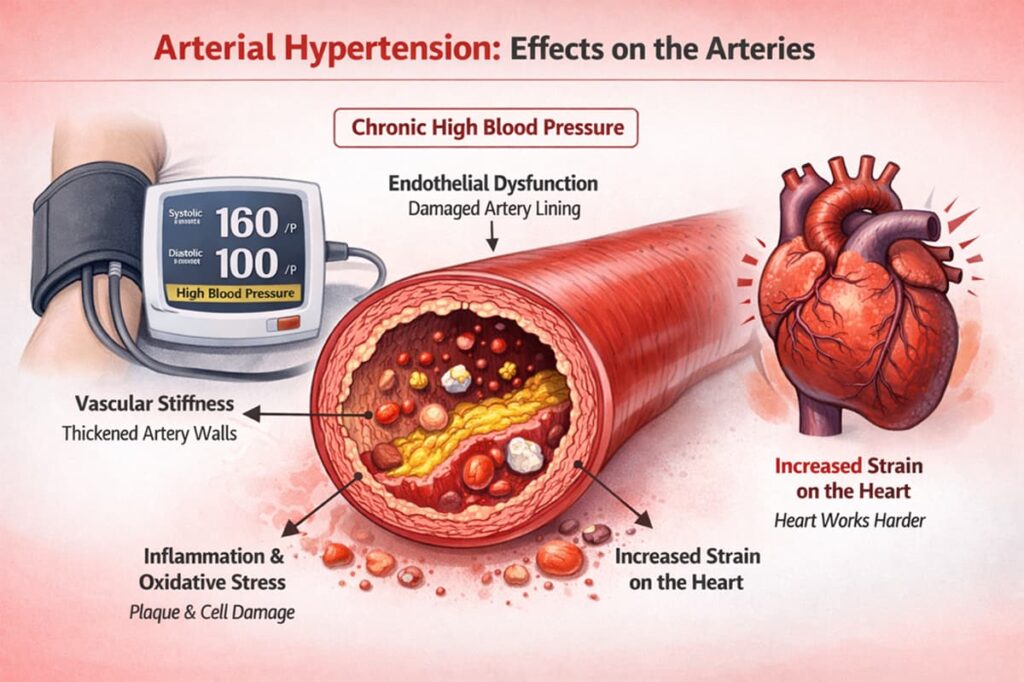
When blood pressure remains elevated over time, it initiates a self-perpetuating process: the vessels gradually lose normal function and elasticity, vascular resistance increases, and blood pressure rises further. Regardless of the original cause, chronically elevated blood pressure itself becomes a major risk factor for damage to vital organs, including the heart, brain, kidneys, and eyes.
High blood pressure is extremely common worldwide and often asymptomatic at first, which is why it’s sometimes called a “silent” condition. Doctors diagnose hypertension based on multiple readings, and they stage it by severity to guide treatment. In everyday practice, if your blood pressure is persistently high, your doctor will discuss a plan to bring those numbers down and protect your health.
Primary vs. Secondary Hypertension
Not all high blood pressure has the same origin. In fact, hypertension is categorized into two main types:
Primary (essential) hypertension—also known as hypertensive disease—is a condition in which persistently elevated arterial blood pressure is the main and defining clinical feature. It accounts for approximately 95% of all cases. Its development is thought to involve multiple contributing factors, including:
- genetic predisposition
- lifestyle factors
- chronic stress
However, no single factor can be identified as a specific cause. For this reason, primary hypertension is regarded as an independent disease rather than a consequence of another underlying condition.
- Secondary hypertension occurs when elevated blood pressure develops as a result of an underlying disease with an identifiable cause. In such cases, the cause can usually be determined through diagnostic evaluation.
Arterial vs Pulmonary Hypertension: Key Differences
When most people say “high blood pressure,” they mean pressure in the main arteries that carry blood from the heart to the whole body—so it affects organs like the brain, kidneys, and heart.
Pulmonary arterial hypertension (PAH) is different. Here, in early stages, the pressure is high in the blood vessels inside the lungs. This makes it harder for blood to pass through the lungs, so the right side of the heart has to pump with extra force. Patients often notice shortness of breath, dizziness, or chest discomfort—especially during activity.
Why High Blood Pressure Becomes Chronic
Several biological mechanisms contribute to hypertension’s self-perpetuating nature.
1. Vascular Stiffness and Endothelial Dysfunction
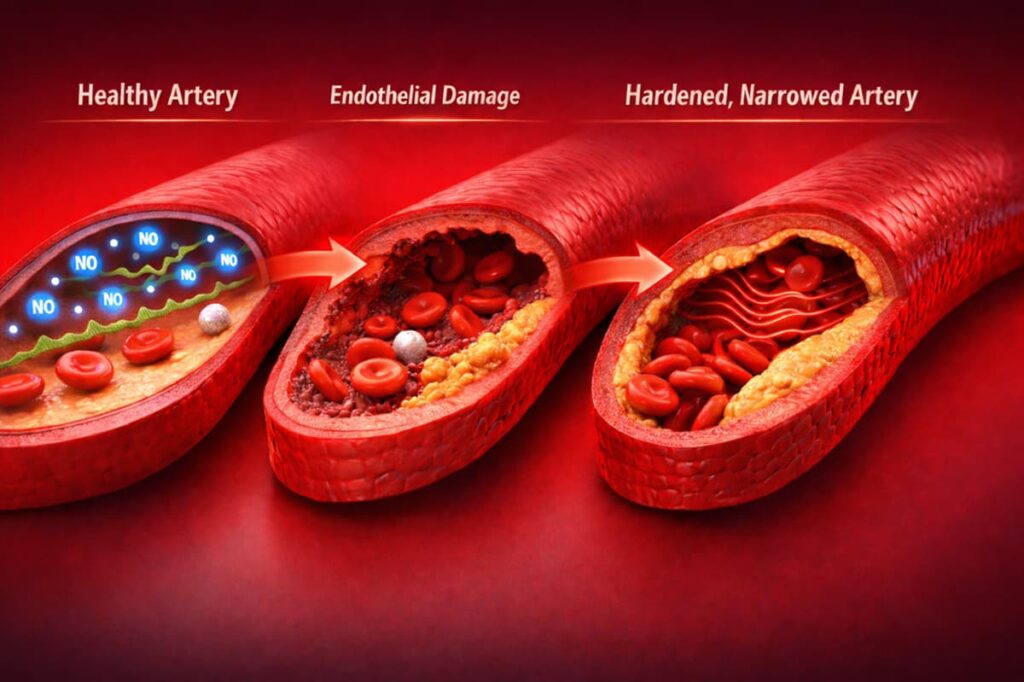
High blood pressure can reinforce itself through changes in the blood vessels. Ongoing pressure damages the inner lining of arteries (the endothelium) and causes the vessel walls to thicken and stiffen. As arteries lose elasticity and their ability to relax, blood pressure rises further—creating a self-perpetuating cycle.
2. Inflammation, Oxidative Stress, and Impaired Microcirculation
There are three key mechanisms through which chronic inflammation contributes to sustained high blood pressure:
- Inflammatory signals promote persistent vessel constriction and further endothelial injury.
- Inflammation also generates oxidative stress—excess reactive oxygen species that can quench nitric oxide and impair the vessels’ ability to relax.
- Damage to the microcirculation narrows small vessels, impairing tissue blood flow and pressure regulation.
For these specific processes, new treatments for high blood pressure are being explored to target the underlying causes of the condition, and stem cell therapy is one of them. We explain this approach in more detail below.
3. Secondary Causes Worth Evaluating
When blood pressure stays high despite treatment, doctors look for an underlying cause that can be corrected. Kidney problems, certain hormone disorders, and conditions like sleep apnea can all keep blood pressure elevated. Finding and treating the root cause often makes blood pressure much easier to manage.
Symptoms, Risks, and Why Blood Pressure Control Matters
Here are the primary symptoms and risks for patients:
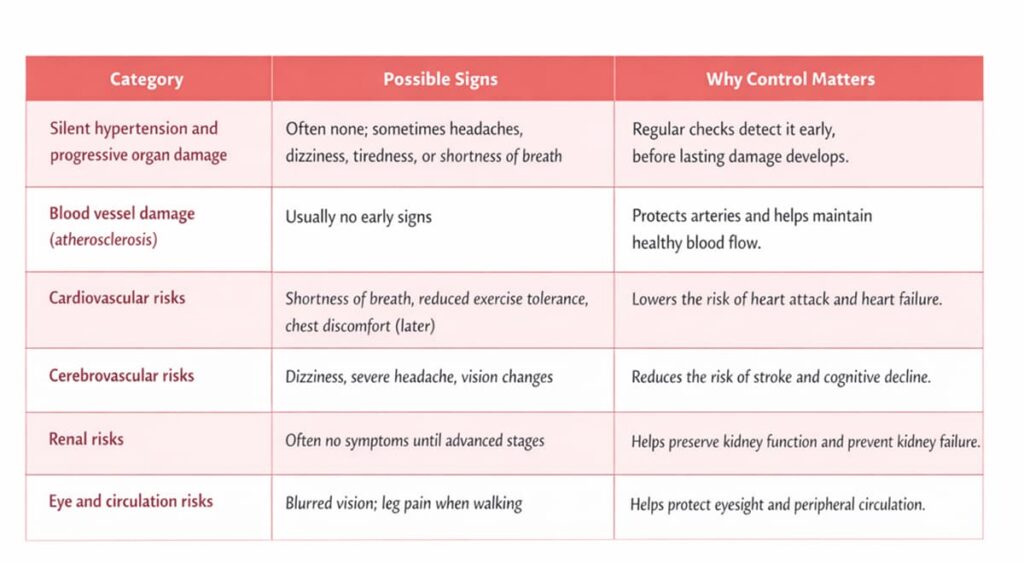
Red Flags Requiring Urgent Care
A sudden or extreme rise in blood pressure can quickly affect vital organs. Symptoms like chest pain, vision loss, weakness, confusion, or a severe headache require immediate medical attention to prevent serious harm.
What Are Effective Treatments for High Blood Pressure Today?
Treating hypertension effectively usually requires a multi-pronged approach.
Lifestyle Measures With Proven Impact on Blood Pressure
Lifestyle modifications are the first and most essential interventions to control high blood pressure. Eating less salt, staying active, keeping a healthy weight, limiting alcohol, and avoiding smoking all help reduce strain on blood vessels. Managing stress and getting enough sleep also support healthier blood pressure over time.
Antihypertensive Medications
When lifestyle adjustments alone aren’t sufficient to reach your target blood pressure, doctors will prescribe antihypertensive medications. There are several types of blood pressure medications that should be prescribed by a doctor, each with a different mechanism of action.
Resistant Hypertension and Next-Step Management
When blood pressure stays high despite several medications, doctors review all drugs and supplements that might interfere with treatment. New treatments for hypertension may be considered when standard therapy is not enough. Along with adjusting medications, specialists may evaluate stem cell treatments for hypertension.
Alternative Treatment for Hypertension: Why Regenerative Medicine Is Being Studied
Given the complex nature of hypertension, scientists are continually seeking alternative treatments for high blood pressure. One such avenue is regenerative medicine—including stem cell therapy—as an adjunct approach for hypertension cases.
The Vascular Target: Endothelium and Arterial Wall Health
Stem cells, especially mesenchymal stem cells (MSCs), have shown promise in repairing tissues by fostering regeneration. In vascular terms, they have the potential to create a more supportive environment for arterial wall and endothelium regeneration.
This is how mesenchymal stem cells for high blood pressure help with vascular recovery through several steps:
- Enter the bloodstream and migrate toward areas of vascular inflammation and injury.
- Respond to chemical signals released by stressed or damaged arteries.
- Release signaling molecules that help reduce inflammation and support endothelial repair.
MSC therapy can be used as an alternative treatment for hypertension, helping to improve arterial flexibility and support better blood pressure control in addition to standard treatment. It may help prevent more serious organ complications.
Discover how stem cells work in heart failure and how they contribute to the formation of new blood vessels in the heart.
Read moreProposed Mechanisms: Anti-Inflammatory, Pro-Angiogenic, Immunomodulatory
Studies and clinical practice showed several mechanisms by which MSCs could positively impact the cardiovascular system.
| Proposed mechanism | How it may support hypertension management |
| Anti-inflammatory effects | MSCs release signaling molecules that reduce chronic inflammation in blood vessel walls, which may lessen vasoconstriction and vascular injury associated with high blood pressure. |
| Pro-angiogenic effects | MSCs secrete growth factors that support the formation of small blood vessels, potentially improving microcirculation in organs affected by long-standing hypertension. |
| Immunomodulation | MSCs can shift immune activity toward a more regulated state, reducing immune-driven vascular damage linked to persistent high blood pressure. |
The goal of this alternative treatment for high blood pressure is not to produce an immediate reduction in blood pressure but to support the cardiovascular system in a way that conventional therapies don’t—by addressing the disease at a more fundamental level.
In our article, we’ll explain the main mechanism of how stem cells for high blood pressure and other chronic conditions work.
Read moreCan Stem Cells Cure High Blood Pressure?
Vascular “repair” does not mean restoring arteries to a disease-free state but supporting their function by improving endothelial health, vessel flexibility, and cellular balance. MSCs may help stabilize damaged vascular tissue and promote healthier vessel behavior, which can make blood pressure easier to manage. Stem cell therapy is used to complement—not substitute—conventional care for a condition shaped by multiple long-term factors.
Beyond cardiovascular conditions, regenerative medicine is also being explored in neurological disorders, including amyotrophic lateral sclerosis (ALS).
Learn more about stem cell therapy for ALS.
How Stem Cell Therapy for Hypertension Is Typically Performed
At Swiss Medica, a stem cell center in Serbia, we have more than 14 years of experience treating chronic conditions using protocols aligned with European standards. The procedure for stem cell treatment for high blood pressure typically includes the following steps:
- Cell sourcing: Before the injection, we carefully prepare MSCs in our own GMP-certified laboratory. For arterial hypertension treatment, these can be allogeneic (donor-derived) or autologous (derived from the patient’s own body).
- Administration: The cells are delivered through an intravenous infusion, usually over 30–60 minutes.
- Treatment course: Therapy may involve a single infusion or several sessions over a few days, depending on the individual plan. At Swiss Medica, the course usually lasts for 3–9 days.
Stem cell treatment for high blood pressure is working in parallel with your current regimen, with the aim that eventually your vascular system might be healthier and perhaps require less pharmaceutical support—but that transition, if it happens, is gradual and medically supervised.
Learn more about the different types of stem cells and how they influence treatment outcomes.
Read moreOutcomes Patients Commonly Report After Stem Cell Therapy for Hypertension
At Swiss Medica, patients often reported a range of positive effects following stem cell therapy:
| Area of effect | What patients commonly report |
| Blood pressure control | More stable readings and easier control alongside existing medication |
| Vascular function | Improved circulation, better exercise tolerance, and reduced headaches or dizziness |
| Microcirculation | Warmer extremities, improved physical stamina, and better tissue oxygenation |
| Inflammation and resilience | Reduced inflammation-related symptoms and improved cardiovascular response to physical or emotional stress |
Note: Individual responses vary, and stem cell therapy is used as a supportive approach alongside standard treatment.
Patient Story at Swiss Medica
— Salvatore Vito, USA (Pennsylvania)
“After seeing how stem cell therapy helped my body heal before, I came to Swiss Medica to support my heart and blood vessels. I wanted to improve blood flow and heart strength, and I’m already starting to feel more capacity and energy.”
You can find more reviews on our YouTube channel.
Safety and Side Effects of Stem Cell therapy for High Blood Pressure
Whenever a new treatment for high blood pressure is considered, safety is a top concern. Stem cell therapy with MSCs has been used in many clinical trials for various conditions and so far has shown a good safety profile.
At Swiss Medica, we pay close attention to each detail. We closely monitor our patients’ vital signs both during and after the stem cell infusion, including blood pressure, heart rate, breathing, and oxygen saturation.
Reported side effects are usually mild and short-lived, most often including low-grade fever, temporary fatigue, headache, nausea, or minor soreness at the injection or IV site, resolving without lasting effects.
Who May Consider Stem Cell Therapy for Hypertension
Stem cell treatment for hypertension may be considered for selected patients based on the following criteria:
| May consider therapy | Generally not suitable |
| Patients with mild, moderate, or resistant hypertension seeking additional vascular support | Patients with uncontrolled infections or severe, uncontrolled chronic diseases |
| Those with hypertension and vascular or metabolic complications (heart disease, kidney involvement, diabetes) | Those with active cancer or recent cancer treatment |
| Patients in stable overall health who are willing to continue standard medical care | Women during pregnancy or breastfeeding period |
Get a free online consultation
If you are considering stem cell therapy, you can leave your contact details below. Our doctors will arrange a free online consultation to review your case carefully and discuss realistic expectations and possible outcomes.

Medical Advisor, Swiss Medica doctor
Stem Cell Therapy for Hypertension: What’s Included in the Swiss Medica Treatment Plan
At Swiss Medica, stem cell therapy is delivered as a structured program, not a single procedure, with the goal of safely supporting blood pressure control and overall cardiovascular health.
1. Diagnostic Assessment and Cardiovascular Review
Our doctors conduct a thorough evaluation of the patient’s health status. This includes a detailed review of your medical history, current medications, and the progression of the hypertension. We may require tests like an electrocardiogram (ECG) or echocardiography to look at heart function, as well as Doppler ultrasounds to assess blood flow in key arteries. The goal is to gain a comprehensive understanding of the patient’s condition and any associated issues.
2. Individualized Regenerative Protocol and Supportive Treatments
Based on diagnostic findings, our medical team designs a personalized regenerative protocol for each patient. This includes selecting the appropriate type of stem cells, defining the dose and treatment schedule, and, when appropriate, integrating supportive options:
- Physiotherapy and kinesiotherapy: Guided movement and physical therapy sessions aimed at improving circulation, supporting cardiac function, and maintaining safe physical activity levels.
- Platelet-rich plasma (PRP): A concentration of the patient’s own platelets used to deliver growth factors that support tissue repair and vascular recovery.
- Exosome therapy: Uses cell-derived signaling particles that may help regulate inflammation and support cellular communication involved in vascular repair.
- IV laser blood irradiation: A technique in which blood is exposed to specific light wavelengths to improve blood flow properties and reduce inflammatory activity
- Intracellular Metabolism Recovery (IMR): A targeted combination of vitamins and metabolic compounds to support overall health.
Learn more about IMR therapy, designed to support vascular regeneration and enhance overall treatment effects.
Read more3. Supportive Environment and Follow-Up
Patients choose Swiss Medica for the following reasons:
Beyond cardiovascular conditions, regenerative medicine is also being explored in neurological disorders, including amyotrophic lateral sclerosis (ALS).
Learn more about stem cell therapy for ALS.
- Experience with cardiovascular and systemic diseases: Our medical team has 14+ years of experience working with chronic cardiovascular conditions, including arterial hypertension, vascular dysfunction, and cardiometabolic disorders.
- Individualized treatment planning: Each protocol is tailored to the patient’s cardiovascular profile, medical history, comorbidities, and current clinical status.
- In-house GMP laboratory: Stem cell processing is performed in our own GMP-compliant lab, ensuring consistent quality, safety, and adherence to European standards.
- Comprehensive care for international patients: We provide coordinated care, including airport transfers, accommodation in our modern hospital, translation support, and balanced medical nutrition.
- Continuous monitoring: We do not just discharge patients after the main course. Our doctors provide a summary report and recommendations and stay in touch at 3–6 months after the therapy to monitor the improvements.
Cost and Accessibility of Stem Cell Therapy for Arterial Hypertension
The cost of stem cell therapy for hypertension varies depending on the treatment protocol, cell type, and clinic location and may range from approximately $30,000 to $35,000 in some settings.
How much do stem cell injections cost at Swiss Medica? We offer treatment programs at a more accessible price point, typically between €7,000 and €31,000*.
*Prices are indicative and based on 2026 estimates; they may vary depending on condition severity and required cell quantity.
How to Start a Consultation
If you’re considering stem cell therapy for high blood pressure, the first step is a free, no-obligation consultation with the Swiss Medica medical team, where you can share your medical history, current blood pressure readings, and medications and discuss whether this supportive treatment may be appropriate for you.
Send a request
If you’re ready to explore your options, book a consultation now and speak directly with a medical specialist.

Medical Advisor, Swiss Medica doctor
Frequently Asked Questions
1. Can stem cells cure high blood pressure?
No—stem cell therapy does not cure hypertension, but it may support vascular health and help some patients achieve better long-term control alongside standard treatment.
2. Can it replace blood pressure medication?
No—medications remain necessary, though in some cases improved blood pressure control after stem cell therapy may allow careful dose reduction under medical supervision.
3. How long do potential effects last?
Improvements may develop over the first 3–6 months and can persist longer, depending on individual response and continued standard care.
List of References:
Carey RM, Moran AE, Whelton PK. Treatment of Hypertension: A Review. JAMA. 2022 Nov 8;328(18):1849-1861. doi.org/10.1001/jama.2022.19590
Fulin Yan,Weishan Wu,Mengxiong Luo,Sidian Yang,Jiguang Yin,Xiangpeng Wang,Effects of Blood Pressure and Antihypertensive Drugs on Rheumatoid Arthritis: A Mendelian Randomization, Network Pharmacology, and Experimental Validation, International Journal of General Medicine, Volume 19, (1-22), (2026). https://doi.org/10.2147/IJGM.S575696
Guo, Y., Yu, Y., Hu, S. et al. The therapeutic potential of mesenchymal stem cells for cardiovascular diseases. Cell Death Dis 11, 349 (2020). https://doi.org/10.1038/s41419-020-2542-9
Wang, Y., Yi, H. & Song, Y. The safety of MSC therapy over the past 15 years: a meta-analysis. Stem Cell Res Ther 12, 545 (2021). https://doi.org/10.1186/s13287-021-02609-x
MD, Pediatrician, Regenerative Medicine Specialist









