Asthma is a chronic inflammatory disease of the airways that affects millions worldwide. While many patients manage asthma well with standard medications, some continue to investigate how to improve long-term control and stability. This need has led to interest in new treatments for asthma that may help address underlying inflammation alongside standard care.
One emerging option is stem cell treatment for asthma, a regenerative therapy approach. This treatment is not a cure or a substitute for regular medications. Instead, it is a supportive strategy that aims to modulate the immune system, reduce chronic inflammation, and promote recovery in the airways.
Understanding Asthma as a Chronic Inflammatory Disease
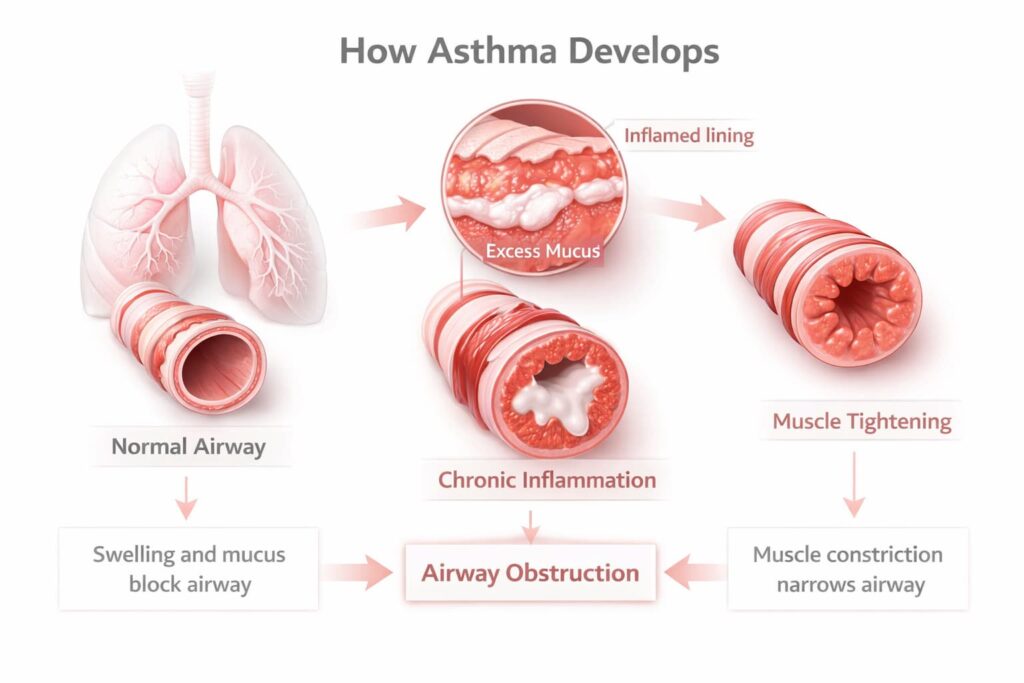
Asthma, also known as bronchial asthma, is characterized by persistent inflammation in the bronchial tubes (airways) that transport air into and out of the lungs.
What Happens in The Airways During Asthma
Bronchial asthma develops due to a combination of inherited traits and environmental factors like allergens, infections, or harmful substances. When the airways come into contact with a trigger, the immune system causes long-term inflammation in the airways.
Chronic Inflammation, Airway Hyperreactivity, and Remodeling
Over time, ongoing inflammation makes the airways more sensitive, keeping them in a hyperreactive state in which even small amounts of the same triggers can provoke a strong response. This process leads to structural changes in the airway walls—known as airway remodeling—including wall thickening and reduced flexibility. As a result, the airways narrow more easily and asthma symptoms occur more frequently.
Why Symptoms Can Persist Despite Treatment
Most asthma medications reduce inflammation or relax airway muscles, and they work well for many patients. However, inflammation may follow pathways that are unresponsive to steroids, or airway remodeling may be advanced. As a result, symptoms can continue despite high-dose inhalers, biologics, or long-term steroid use—prompting interest in additional alternative therapies for asthma.
Conventional Asthma Treatments and Their Limitations
Standard asthma treatments are essential for controlling symptoms, but they don’t address all aspects of the disease.
| Aspects of Treatment | What It Does | Key Limitations |
| Inhaled therapies | Reduce airway inflammation and relax airway muscles to control daily symptoms | Symptoms often return if treatment is stopped; does not reverse long-term airway changes |
| Biologic medications | Target specific immune pathways in severe asthma (e.g. allergic or eosinophilic asthma) | Effective only for certain patients; require long-term use and regular injections |
| Steroid therapy | Strongly suppresses airway inflammation during flares or severe disease | Long-term use can cause significant side effects; some patients become steroid-dependent or resistant |
Why Inflammation and Airway Remodeling May Persist
Steroids and other medications help control symptoms but generally do not change long-term structural changes in the airways, like thickening or scarring caused by years of inflammation. Symptoms can return when medications are reduced or stopped. These limitations are the reason why researchers are exploring alternative asthma treatments that aim to address underlying inflammation and modulate immune system response.
Alternative Asthma Treatments: Why Regenerative Therapies Are Being Explored
Researchers are exploring new treatments for asthma beyond the traditional medications. One promising avenue is mesenchymal stem cells in regenerative medicine (MSCs), which have shown excellent safety records and possible benefits in helping the immune system and repairing tissue in inflammatory conditions.
Immune Modulation of Overactive Responses
Asthma often involves an overactive immune response. Regenerative therapy uses MSCs to modulate the immune system, turning down the overreaction. Unlike drugs that focus on a specific pathway, stem cells act on multiple immune pathways at once.
Reducing Chronic Airway Inflammation
MSCs release special molecules—growth factors, chemokines, and adhesion molecules—that can migrate to inflamed lung tissue and reduce inflammation. MSC treatments have been shown to decrease levels of inflammatory cytokines, which are responsible for causing allergy symptoms.
Supporting Lung Tissue Repair and Airway Integrity
MSCs may create supportive environments for airway lining repair and healthier tissue remodeling in lungs affected by chronic inflammation, potentially improving airway stability over time.
Get a free online consultation
At Swiss Medica, we’ve been working with challenging conditions such as asthma and pulmonary fibrosis for over 14 years, helping many patients achieve disease stabilization. We offer free, no-obligation online consultations with our regenerative specialists—if you’re exploring additional ways to support your health, book a meeting in this form.

Medical Advisor, Swiss Medica doctor
How Stem Cell Therapy Works in Asthma
In asthma, stem cell therapies focus on calming abnormal immune activity in the lungs and creating a supportive environment for tissue repair, rather than simply relieving symptoms.
Stem Cells Used to Treat Asthma
Most studies and clinical practices focus on MSCs, which may come from the following sources:
- Donor umbilical cord tissue (allogeneic MSCs)—collected after healthy births and commonly used due to consistent quality and safety.
- Patient’s own tissues (autologous MSCs)—typically obtained from bone marrow or fat tissue. Used only in specific cases.
To better understand where MSCs come from and how they differ from embryonic stem cells, you can read more in our dedicated article.
Read moreAs we mentioned above, MSCs do not replace lung tissue; instead, their signaling molecules create special environments that “wake up” the body’s own resources and help in these processes:
- Reducing Th2-driven inflammation. Immune cells known as Th2 cells overreact in allergic asthma, causing persistent inflammation in the airways. MSCs release signals that help quiet this response, reducing swelling and sensitivity in the lungs.
- Limiting eosinophil activity. Eosinophils are inflammatory cells that can damage airway tissue. MSCs may reduce the signals that attract and activate these cells, helping to lower irritation in the airways.
- Increasing regulatory immune cells. Regulatory immune cells act as natural “controls” that prevent the immune system from overreacting. MSCs can support these cells, helping the immune system respond more evenly.
Administration routes. In current treatment protocols, stem cells for asthma are typically administered by intravenous infusion and inhalation so they can reach the lungs through normal circulation.
For a more detailed, science-based explanation of how MSCs interact with the body and influence immune and tissue pathways, you can explore our dedicated article.
Read moreCan Stem Cells Repair or Support Lung Function in Asthma?
MSC therapy for lung diseases may help repair the airway lining and reduce inflammation, which can support airflow, but it does not reverse permanent structural changes caused by asthma. By limiting ongoing inflammation, it may also help slow further airway thickening and lead to modest improvements in lung function.
Can Stem Cells Cure Asthma?
Stem cell therapy does not cure asthma. Rather, it is a supportive approach that, in conjunction with standard treatments, may help improve control and quality of life, with any medication changes made gradually and under medical supervision.
What Improvements Some Patients May Experience after Stem Cell Therapy for Asthma
Based on early clinical reports and our clinical practice, here are some of the benefits of stem cell injection that patients have shared.
| Potential Benefit | Description |
| Reduced wheezing, tightness, and shortness of breath | MSC-based approaches can help patients breathe easier. |
| Fewer exacerbations and flare-ups | MSC therapy may make respiratory symptoms less reactive over time, leading to fewer acute episodes. |
| Potentially reduced reliance on systemic steroids | Due to their broad immunoregulatory effects, MSC therapy may reduce the need for certain symptom-relief treatments. The need for and extent of ongoing standard therapy are determined individually and cannot be guaranteed. |
| Improved exercise tolerance and daily comfort | With reduced airway inflammation and tissue stress, patients may experience better tolerance to physical activity and improved daily comfort. |
— A patient from Australia with chronic asthma and eosinophilic pneumonia
“I’ve lived on steroids every eight hours just to breathe—I was out of options. After stem cell therapy at Swiss Medica, I could breathe through my nose for the first time in years without sprays. That might sound small, but for me, it was a turning point. I finally felt the inflammation ease.”
Note: Individual results vary.
Who May Be a Suitable Candidate for Stem Cell Treatment for Asthma
Stem cell therapy for asthma is not a universal solution. The main criterion is the patient’s overall health rather than the diagnosis itself; it is best suited to people with mild asthma and related conditions.
| May Be Considered | May Not Be Suitable |
| The main criterion is the patient’s overall health rather than the diagnosis itself; it is best suited to people with mild asthma and related conditions. | Active infections (e.g., pneumonia, tuberculosis) |
| Stable general health apart from asthma | Severe organ failure (e.g., cardiac or renal) increasing infusion risk |
| History of multiple hospitalizations or rescue inhaler use despite medications | Pregnancy |
Stem Cell Treatment for Asthma at Swiss Medica: Personalised Program Tailored to Your Needs
At Swiss Medica, a world stem cell clinic in Serbia, we offer a structured, patient-centered program for stem cell therapy for asthma. Here’s what you can expect from our personalized regenerative program.
Detailed Diagnostics
Your program starts with an assessment of breathing function and current asthma control, including spirometry with a bronchodilator test. When clinically indicated, additional tests may include inflammation markers, allergy evaluation, or high-resolution chest imaging. Based on these results, we determine whether stem cell therapy is appropriate for your case and how to tailor it effectively.
Personalized Regenerative Protocol
Based on your diagnostic results, we create a tailored treatment plan using MSCs. We adjust the cell type, dose, and number of infusions to suit your individual condition.
Supporting Modalities
To enhance the effects of stem cell therapy, the program may include:
- Physiotherapy and kinesiotherapy.
- Medical device treatments like electrotherapy, ultrasound, lymphatic drainage, or low-level laser therapy.
- Intracellular Metabolism Recovery (IMR) procedures—a personalized mix of vitamins, minerals, amino acids, and antioxidants to support lung function and overall recovery.
- Plasmapheresis (in some specific cases)—a procedure that filters the blood to remove harmful antibodies and toxins.
These supportive therapies may help prepare the body and improve how it responds to treatment.
Treatment Timeline and Patient Experience
From your first day at the clinic, we stay involved—not just to deliver treatment, but to monitor your response and support your recovery.
- Length of stay: Most patients spend 3–9 days with us, depending on the treatment plan.
- When to expect changes: Some patients notice early shifts—like fewer symptoms or easier breathing—in the first month, but most progress becomes clearer in 3–6 months.
- Medications still matter: Keep using your regular asthma treatments unless your doctor decides to adjust them later. Stem cell therapy adds to your regimen—it doesn’t replace it right away.
- Staying connected: After you leave, we check in at 3–6 months. You’ll have a detailed medical summary, and our team stays available if you have questions or need advice.
Safety and Clinical Evidence for Stem Cell Therapy for Asthma
MSC therapy has demonstrated a strong safety profile across multiple clinical trials involving lung diseases. Stem cells are considered hypoimmunogenic, meaning they are unlikely to provoke immune rejection. Studies show MSCs’ effectiveness:
- A 2023 case report of a 68-year-old patient with uncontrolled asthma showed marked improvement after receiving a single infusion of MSCs: over 90% reduction in rescue inhaler use and sustained symptom improvement over six months, with no adverse events reported during follow-up.
- A review from 2022 highlights MSCs as a serious candidate for future asthma management, especially for patients with persistent inflammation and airway remodeling despite standard treatments.
Possible Side Effects and Risk Management in Stem Cell Therapy for Asthma
Most patients tolerate stem cell therapy for asthma very well, but like any medical procedure, it can involve temporary and short-term side effects:
- Low-grade fever or chills
- Mild headache or nausea
- Temporary fatigue
- Local irritation or bruising at the IV site
At Swiss Medica, patient safety is integrated into every stage of care. All individuals are medically screened to confirm suitability before treatment begins, and every therapy is carried out under close clinical supervision. Our stem cells for asthma are processed in-house in a GMP-certified laboratory under strict supervision. This internal production system allows us to oversee quality and safety from the lab to the infusion room.
Why Patients Choose Swiss Medica
Patients with asthma and other chronic conditions trust Swiss Medica not only for our clinical expertise but also for the depth of personalized care we provide throughout every step of the treatment journey. Here’s what sets us apart:
- Medical expertise with focused experience. We focus on regenerative medicine and have an 80% success rate in treating complex conditions like asthma, COPD, and autoimmune disorders.
- Individualized treatment plans. No two patients receive the same program—your therapy is tailored to your clinical profile, goals, and health needs.
- Multidisciplinary team. Care is provided by specialists in neurology, cardiology, and rehabilitation, working together to address each patient’s needs comprehensively.
- Modern clinical infrastructure. We operate fully equipped, medically certified facilities with in-house laboratories and diagnostics, combining medical precision with a quiet, restorative setting.
- International patient coordination. We’ve supported patients from over 70+ countries with translation, airport pickup, comfortable accommodations, and medically appropriate meals.
- Transparent results and long-term support. We maintain clear outcome reporting and offer continued access to our team even after you return home, ensuring ongoing support and guidance.
Our newly built medical center functions as a fully equipped hospital, offering inpatient care, diagnostic imaging, and 24/7 monitoring.
What Is the Cost of Stem Cell Therapy for Asthma?
The stem cell therapy price isn’t one-size-fits-all—it depends on the medical condition being treated, the number and source of stem cell infusions, the complexity of your case, and any additional therapies or diagnostics involved.
| Region | Estimated Cost of Stem Cell Therapy for Asthma and Other Conditions |
| USA | $15,000–$40,000+ |
| Europe | €12,000–€35,000 |
| Serbia (Swiss Medica) | €7,000–€31,000* |
*Prices are indicative and based on 2026 estimates; they may vary depending on condition severity and required cell quantity.
In Europe and the USA, regenerative treatments are either restricted to clinical trials or priced well beyond reach. As a result, patients often explore options for stem cell therapy abroad—but affordability alone should never come at the cost of medical safety. At Swiss Medica, we combine international clinical standards with individualized care programs at more accessible rates, making regenerative therapy for asthma a transparent and structured option.
How to Start a Consultation
Swiss Medica offers free consultations to help you explore whether stem cell therapy for bronchial asthma is a suitable option for you; it’s a chance for our doctors to evaluate your case thoroughly and for you to gain clear insight into potential outcomes—without any financial commitment.
Contact us
If you’re considering stem cell treatment for asthma, we invite you to begin with a free online consultation—no pressure, just an honest conversation about whether this treatment could be right for you. Start your free consultation today.

Medical Advisor, Swiss Medica doctor
Frequently Asked Questions
1. Are stem cells an alternative cure for asthma?
Patients often wonder, “Can stem cells cure asthma if they have the potential to create a unique environment for recovery?” Stem cell therapy is not a cure for asthma but may work as a supportive treatment to help reduce inflammation and improve long-term control.
2. Can stem cell therapy for bronchial asthma replace inhalers or biologics?
Stem cell therapy complements standard treatments and should not replace them without medical supervision.
3. How long might benefits last?
Benefits from stem cell therapy may last from 3–6 months to 1 year, but results vary between individuals.
4. Can I bring a caregiver or family member with me?
We encourage patients to bring a caregiver or companion, and we’ll gladly help arrange accommodation and support during your stay.
List of References:
Xiu Yu and Li Yu and Bingxin Guo and Rongchang Chen and Chen Qiu, A narrative review of research advances in mesenchymal stem cell therapy for asthma. Annals of Translational Medicine, 2020 https://atm.amegroups.org/article/view/55089
Wang, Y., Yi, H. & Song, Y. The safety of MSC therapy over the past 15 years: a meta-analysis. Stem Cell Res Ther 12, 545 (2021). https://doi.org/10.1186/s13287-021-02
Abbaszadeh, H., Ghorbani, F., Abbaspour-Aghdam, S. et al. Chronic obstructive pulmonary disease and asthma: mesenchymal stem cells and their extracellular vesicles as potential therapeutic tools. Stem Cell Res Ther 13, 262 (2022). https://doi.org/10.1186/s13287-022-02938-5
Sharan J, Barmada A, Band N, Liebman E, Prodromos C. First Report in a Human of Successful Treatment of Asthma with Mesenchymal Stem Cells: A Case Report with Review of Literature. Curr Stem Cell Res Ther. 2023;18(7):1026-1029. doi.org/10.2174/1574888X18666221115141022
MD, Pediatrician, Regenerative Medicine Specialist











